
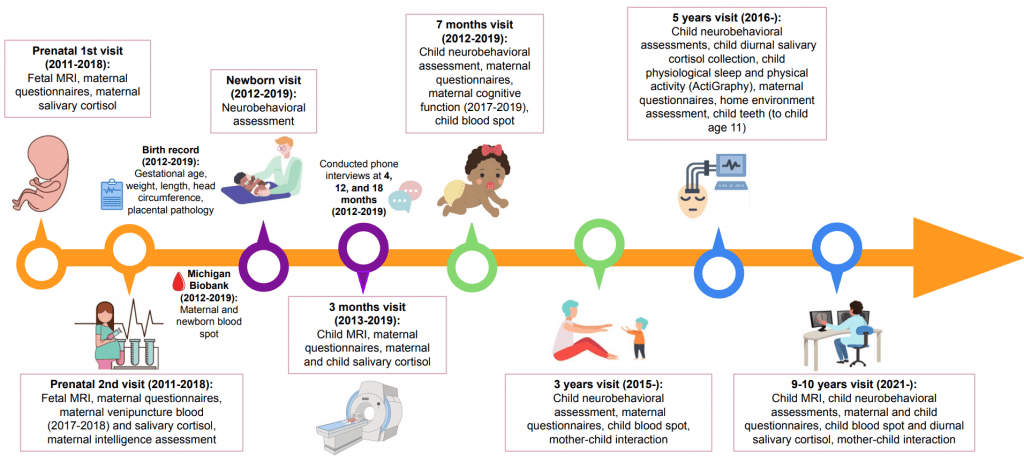
This longitudinal study is made up of multiple waves of data collection examining the neurodevelopmental progression of self-regulatory behavior and emotion competence, starting at the very beginning of life by evaluating in utero brain functional connectivity.
We focus on the child and mother to ultimately explore the healthy neurodevelopment of children and fetuses; bases for cognitive control, emotion regulation, and the development of psychopathology; the connectivity of functional networks in the developing brain; and other factors that influence variation in pediatric neurobehavioral development.
We aim to link measures of child health back to prenatal factors, such as fetal brain connectivity and maternal psychological stress.
Perinatal Imaging of Neural Connectivity
pregnancy & infancy

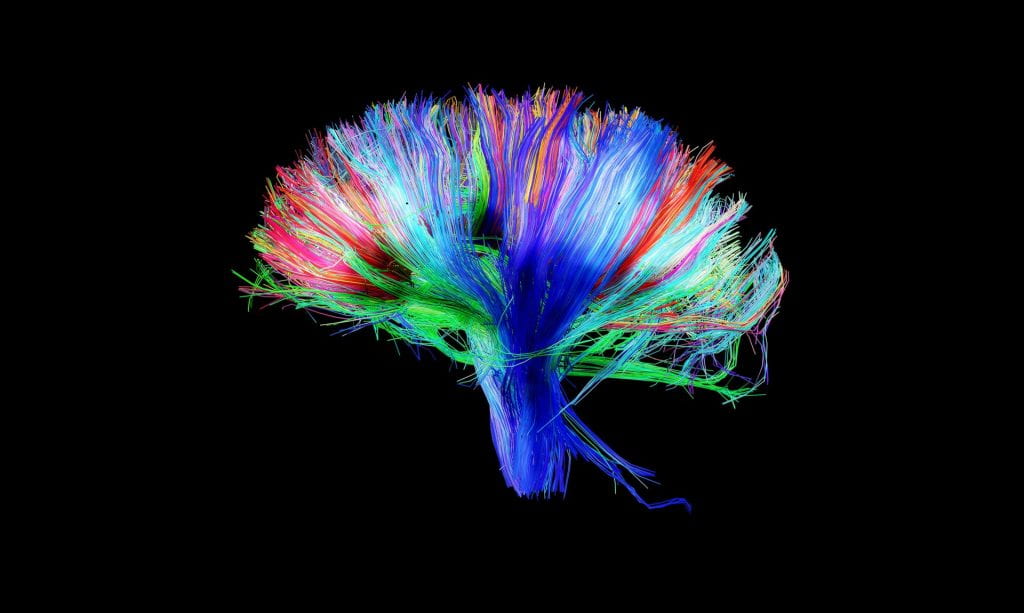
Following the recruitment of expecting mothers, the first wave of data acquisition, which was led by Dr. Moriah Thomason, involved functional (resting-state) and structural (diffusion tensor) neuroimaging methods of the human fetus to model healthy and atypical brain development in utero. We aimed to establish the sequence and patterning of fetal functional neural networks.
Prior to entering the MRI scanner, the mother completed a number of questionnaires to assess aspects of her emotional and physical state, including her mental and physical health, socioeconomic status, and attachment style.
In addition to these tasks, maternal salivary cortisol samples and maternal blood samples were collected.
Following this visit, we then further mapped the emergence of the human connectome by inviting mothers back with their child after giving birth. Here, infants were studied during natural sleep using resting-state, diffusion tensor (DTI), and functional MRI tasks (passive processing of emotional non-words, exposure to maternal smell). Mothers completed various questionnaires, and infant salivary cortisol samples were collected at this visit.
Early Life Risk, Resilience, and Behavioral Outcomes
age 7 months, 36 months

Mom and child were invited back to the lab when the child reached seven months old, and again once the child reached 36 months old.
During the seven-month visit, the mother and child engaged in the Still-Face Paradigm to assess child socioemotional regulation.
During the 36-month visit, the mother-child dyad completed interactive tasks. Dr. Marjorie Beeghly’s team codes these tasks using an adaptation of the Parent-Child Interaction System (PARCHISY).
During both visits, the Bayley Scales of Infant Development were completed to assess child developmental functioning. At both visits, mothers completed questionnaires that include measures of infant behavior, parenting experiences, health, and life circumstances.
Child cortisol, height, weight and blood spots were also collected.
Early Childhood Neurodevelopmental Health Outcomes
age 5 years
We are in the process of following up with children when they reach 5 years of age.
During an initial home visit, we assess the sleep environment, provide an ActiGraph wristband for the child to wear for the measurement of child sleep and physical activity, and deliver diurnal cortisol sample collection materials for the mother to collect from her child. We also interview the mother during this visit to assess her child’s traumatic experiences.
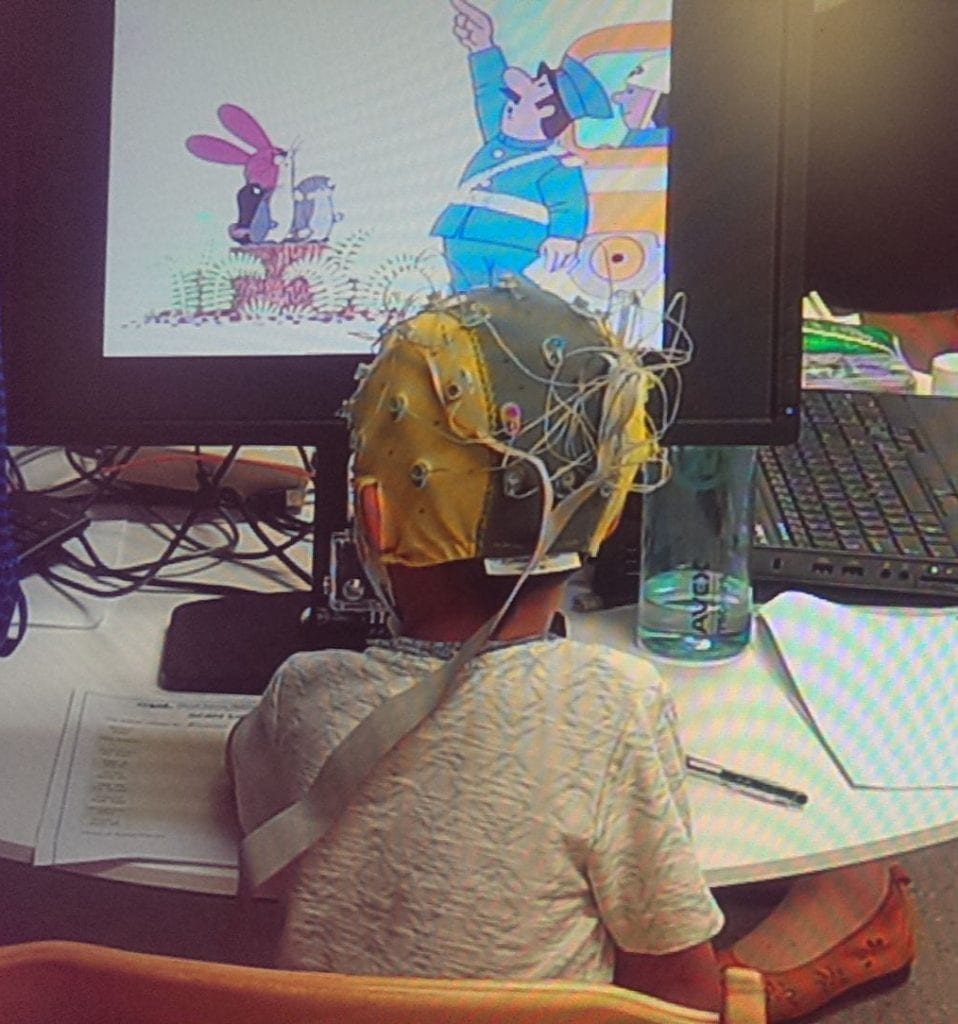
The mother and child then participate in another lab visit. Here, a number of measures are completed including child height, weight, and assessments of school readiness and emotion regulation. Mother-child interaction is also recorded. The child also completes several computer tasks to measure executive functioning and additional tasks to measure emotion regulation with electroencephalography (EEG).
The Tooth Fairy Project
age 3 — 11 years
We collect naturally shed baby teeth from our longitudinal cohort to assess toxicant and micronutrient exposures and inflammatory markers in collaboration with Dr. Christine Austin and her research team at Mt. Sinai.
Follow-up Assessment of Inflammation and Neurobehavioral Development
age 9 years

Our team recently started another follow-up assessment at age 9-10 years. This wave aims to identify whether inflammation in the human prenatal period exerts influence over the developing fetal neural connectome and subsequently increases risk for problem behaviors and disorders in childhood.
This project involves the pairing of new advances in resting-state functional connectivity MRI with innovations in tooth-biomarker assays using the deciduous tooth samples collected throughout the Tooth Fairy Project. Data collection involves the following:
- An initial home visit in which families are given an ActiGraph wristband to measure child sleep and physical activity as well as a diurnal cortisol collection kit. A child blood sample is also collected. Children additionally complete various neurobehavioral assessments (executive functioning, attention, memory, language development) using tests included in the NIH Toolbox, as well as a matrix reasoning task to assess neurocognition.
- A lab visit that includes a child MRI using the same scanner that was used prenatally. Behavioral observation includes a conflict discussion task between the mother and child.
Throughout both visits, mothers complete a number of questionnaires assessing factors such as her physical health, family cohesion, neighborhood, child’s behavior, maternal depression, maternal anxiety, parenting, maternal perceived stress, and perceived discrimination. Children also complete questionnaires, which include measures of child depression, anxiety, trauma, resilience, behavioral approach, and physical health.
This wave of data collection is intended to be partially harmonized with the NIH Adolescent Brain Cognitive Development (ABCD) Study protocol.
Privacy Policy
The information below refers to the Facebook Ads we employ to increase recruitment.
All information collected about your child during the course of this study will be kept confidential to the extent permitted by law. Your child will be identified in the research records by a code name or number. Information that identifies your child personally will not be released without your written permission. However, the study sponsor, the Institutional Review Board (IRB) at Wayne State University, or federal agencies with appropriate regulatory oversight [e.g., Food and Drug Administration (FDA), Office for Human Research Protections (OHRP), Office of Civil Rights (OCR), etc.) may review your records.When the results of this research are published or discussed in conferences, no information will be included that would reveal your child’s identity. If photographs, videos, or audiotape recordings of you or your child will be used for research or educational purposes, your child’s identity will be protected or disguised. Any videos of you and your child will be stored electronically with a file name that only contains your study ID number. The electronic files are stored in a password- protected file on a password-protected computer. Only the research team will have access to the audio and video file. If you agree, your video file may be used for the purposes you have specified as acceptable after the end of the study. If you do not agree to future use of your videos, they will be destroyed/deleted at the conclusion of the study or after future study extensions. You have the right to review recordings.
Certificate of Confidentiality:
This research is covered by a Certificate of Confidentiality from the National Institutes of Health. This means that the researchers cannot release or use information, documents, or samples that may identify you in any action or suit unless you say it is okay. They also cannot provide them as evidence unless you have agreed. This protection includes federal, state, or local civil, criminal, administrative, legislative, or other proceedings. An example would be a court subpoena. There are some important things that you need to know. The Certificate DOES NOT stop reporting that federal, state or local laws require. Some examples are laws that require reporting of child or elder abuse, some communicable diseases, and threats to harm yourself or others. The Certificate CANNOT BE USED to stop a sponsoring United States federal or state government agency from checking records or evaluating programs. The Certificate DOES NOT stop disclosures required by the federal Food and Drug Administration (FDA). The Certificate also DOES NOT prevent your information from being used for other research if allowed by federal regulations. Researchers may release information about you when you say it is okay. For example, you may give them permission to release information to insurers, medical providers or any other persons not connected with the research. The Certificate of Confidentiality does not stop you from willingly releasing information about your involvement in this research. It also does not prevent you from having access to your own information.
